What is the Diabetes Honeymoon Phase?
The diabetes honeymoon phase, also known as the remission phase, is a period that can occur after the initial diagnosis and treatment of Type 1 diabetes. This phase is characterized by a temporary decrease in the need for insulin and an improvement in blood sugar control. It’s a time when some or all of the symptoms of diabetes may disappear or become less severe. However, it’s important to understand that the honeymoon phase is not a cure for diabetes. It’s a transient period that will eventually end, and the body’s ability to produce insulin will continue to decline.
Understanding the Onset of Type 1 Diabetes
Type 1 diabetes is an autoimmune disease where the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. This means the body is unable to produce insulin, a hormone essential for allowing glucose (sugar) from food to enter cells for energy. Consequently, glucose builds up in the bloodstream, leading to various health complications. During the initial diagnosis, the immune system is still actively attacking the remaining insulin-producing cells, but some function may remain, leading to a temporary remission.
The Definition and Duration of the Honeymoon

The diabetes honeymoon phase is the period where the body still has some ability to produce insulin. This can lead to lower insulin needs and more stable blood sugar levels. The duration of the honeymoon phase varies greatly from person to person. It can last from a few weeks to several months, or even up to a year or more in some cases. The length of the honeymoon phase depends on several factors, including the individual’s age, how quickly diabetes was diagnosed, the initial treatment plan, and how well they manage their diabetes.
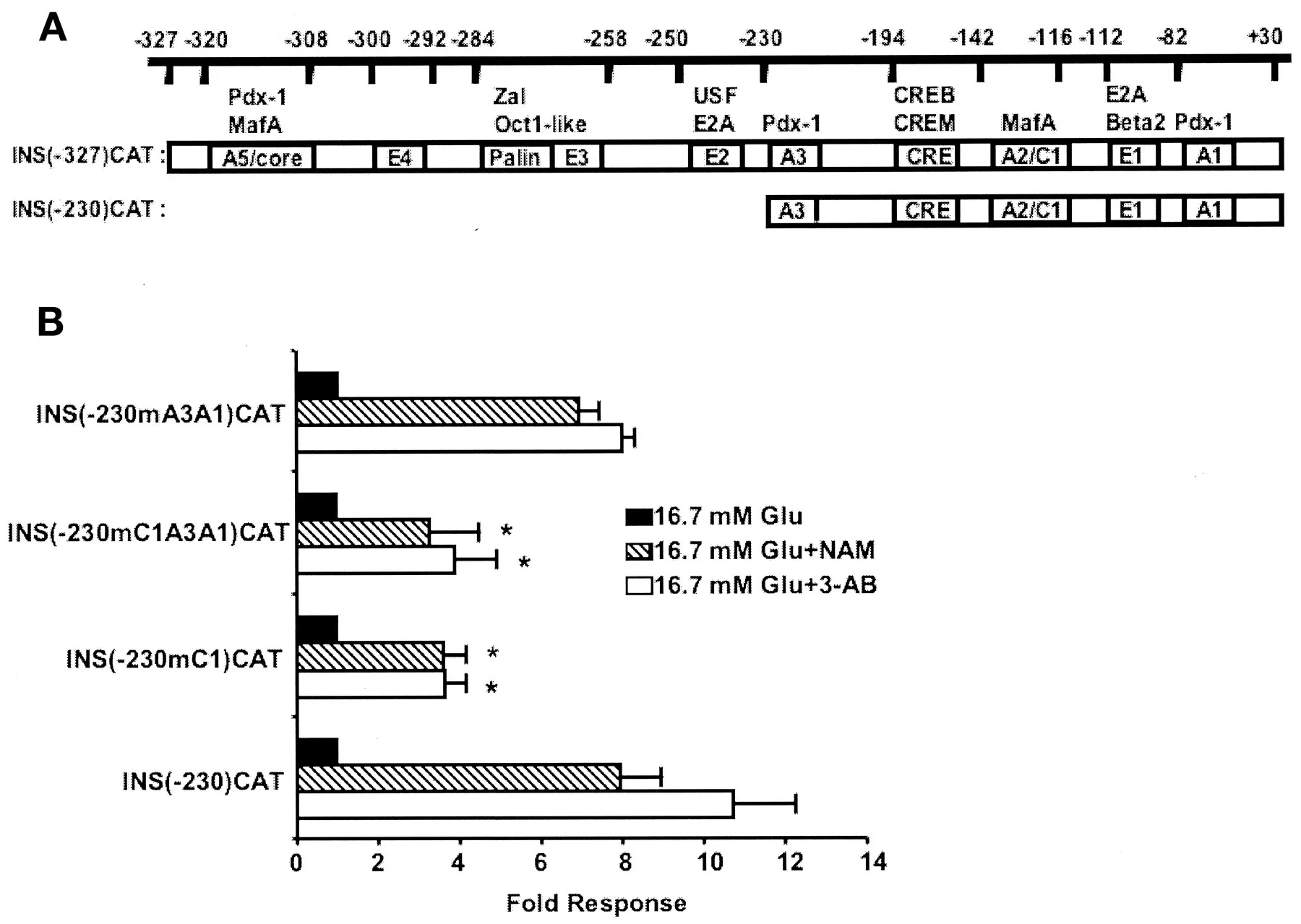
How the Pancreas Functions in This Phase
During the honeymoon phase, the pancreas still has some residual function. While the immune system has destroyed a significant portion of the insulin-producing beta cells, some may still be alive and producing insulin. This remaining insulin production, combined with the effects of initial treatment (such as insulin injections or insulin pump therapy), can lead to improved blood sugar control. This allows the individual to potentially require less insulin or even experience a period where insulin needs are very low. The goal during this phase is to preserve any remaining beta-cell function for as long as possible.
5 Sweet Tips to Extend Honeymoon Phase
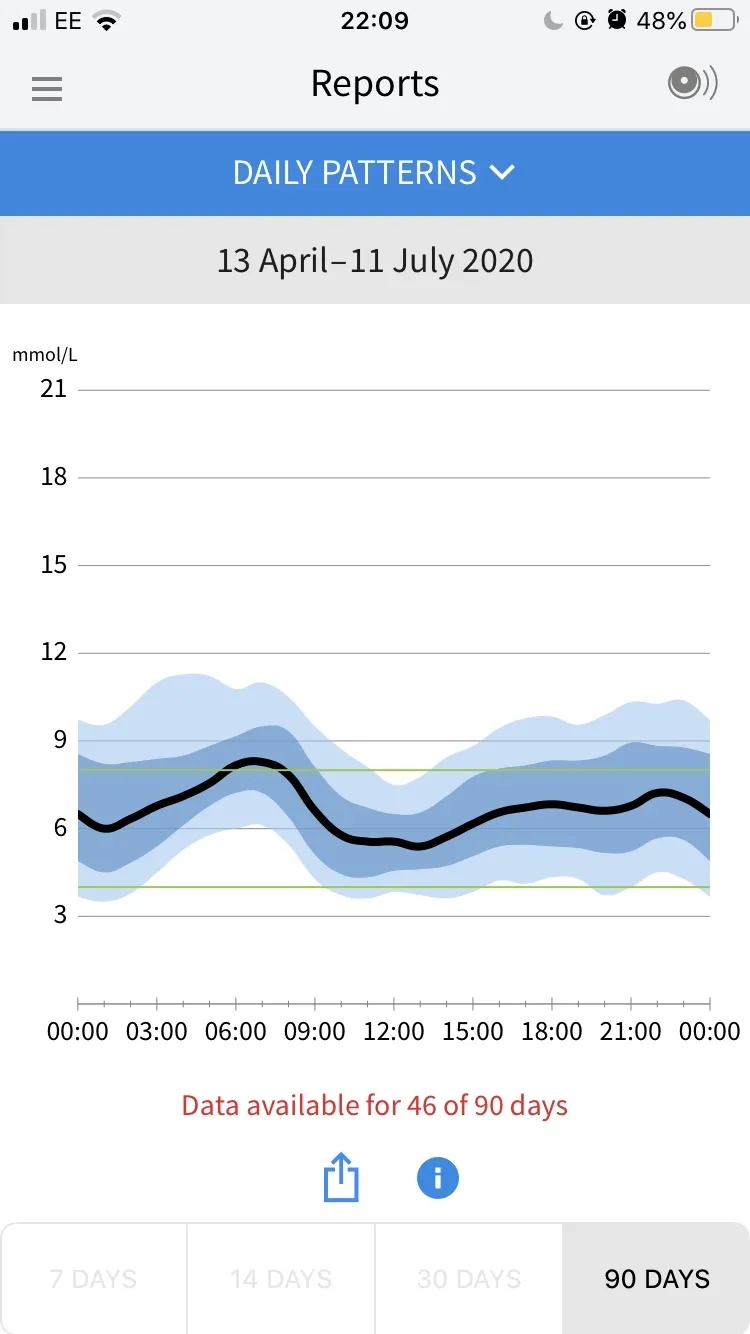
Tip 1 Monitor Blood Glucose Regularly
Regular blood glucose monitoring is crucial to managing diabetes, particularly during the honeymoon phase. Consistent monitoring provides valuable insights into how your body responds to food, exercise, and medication. It allows you to make informed decisions about your insulin dosages and other lifestyle adjustments. Consistent blood sugar monitoring helps you to catch and address high or low blood sugar levels promptly, preventing complications and allowing you to maintain good control. By tracking your levels, you gain a better understanding of your body’s response to various factors.
Understanding the Importance of Regular Monitoring
Monitoring blood glucose levels regularly helps you to see how your body reacts to different factors, such as food, exercise, and stress. It allows you to adjust your insulin dosage and lifestyle accordingly. The data helps to keep your blood sugar within a healthy range, lowering the risk of long-term complications. Additionally, frequent monitoring encourages better overall management, giving you a sense of control over your health. This detailed tracking empowers you to make proactive decisions for better diabetes management.
Best Practices for Glucose Checks
To get accurate results, wash your hands with warm, soapy water and dry them thoroughly before testing. Always use a fresh test strip and a properly calibrated glucose meter. Test your blood glucose at the times recommended by your healthcare team, such as before meals, after meals, before bed, and sometimes during the night. Record your results, along with any relevant information such as food intake, exercise, and medication doses, in a logbook or tracking app. Share these logs with your healthcare team at each check-up to adjust and manage your diabetes.
Tip 2: Follow a Balanced Diet
Diet plays a crucial role in managing diabetes, particularly during the honeymoon phase. A balanced diet can help regulate blood sugar levels, support overall health, and potentially extend the honeymoon phase. Focus on eating a variety of nutrient-rich foods and controlling carbohydrate intake. Partner with a registered dietitian or certified diabetes educator to create a personalized meal plan that suits your individual needs and lifestyle.
The Role of Nutrition in Diabetes Management
Proper nutrition is fundamental in managing diabetes, as it directly impacts blood glucose levels. Carbohydrate intake is a major factor, requiring careful monitoring to avoid spikes and drops. Balanced meals, including proteins, healthy fats, and fiber-rich foods, contribute to more stable blood sugar levels. The right nutrition plan helps to reduce the risk of diabetes-related complications. A well-planned diet complements medication and exercise, creating a holistic approach to diabetes care.
Foods to Embrace and Foods to Limit
Focus on eating whole, unprocessed foods, including non-starchy vegetables (broccoli, spinach), lean proteins (chicken, fish, beans), and whole grains (brown rice, quinoa). Limit your intake of refined carbohydrates (white bread, pastries), sugary drinks, and saturated and trans fats. Choose healthy fats, like those found in avocados, nuts, and olive oil. Pay attention to portion sizes and timing your meals to help manage blood glucose. Make sure to plan your meals ahead of time and keep healthy snacks on hand to avoid unhealthy choices.
Tip 3 Engage in Regular Physical Activity

Physical activity is a key component of diabetes management and can help extend the honeymoon phase. Exercise improves insulin sensitivity, allowing your body to use insulin more effectively. This can lead to lower blood sugar levels and a decreased need for insulin. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, plus strength training exercises at least two days a week. Always consult your healthcare team before starting any new exercise program.
Benefits of Exercise During the Honeymoon
Exercise enhances insulin sensitivity, helping the body to use insulin more efficiently. This means less insulin might be needed to manage blood sugar levels. Regular physical activity aids in weight management, a significant factor in diabetes care. It boosts cardiovascular health and reduces the risk of heart disease, a common concern for people with diabetes. Exercise also improves mood, reduces stress, and can boost overall well-being. This holistic approach contributes to better diabetes management during the honeymoon phase.
Types of Exercises to Consider
Incorporate a combination of aerobic and resistance exercises into your routine. Aerobic exercises include brisk walking, jogging, swimming, and cycling. Resistance exercises involve lifting weights, using resistance bands, or doing bodyweight exercises like push-ups. Find activities you enjoy, and vary them to prevent boredom. Before starting any new exercise routine, consult with your doctor or a certified fitness trainer to make sure the exercises are safe for you. Always monitor your blood glucose levels before, during, and after exercise to understand how your body responds.
Tip 4: Proper Medication Management

Proper medication management is critical for successful diabetes care, particularly during the honeymoon phase. Following your prescribed insulin regimen, and any other medications, is crucial for controlling blood sugar levels and extending the remission period. Understand the types of medications you are taking, their dosages, and the proper administration techniques. Make sure to discuss any concerns or side effects with your healthcare team. Always keep your medication readily available.
Understanding Insulin and Other Medications
Insulin is a key medication for Type 1 diabetes, and there are various types, including rapid-acting, short-acting, intermediate-acting, and long-acting. The type of insulin prescribed depends on your individual needs. Other medications, such as pramlintide, may be used in conjunction with insulin. Understand how each medication works, how it affects your blood sugar, and the potential side effects. Learn the correct way to administer your medications, including the proper injection technique if using insulin pens or syringes.
Dosage, Timing, and Storage
Always follow your doctor’s instructions regarding the dosage and timing of your medications. Use a regular schedule to take your insulin and other medications. If you miss a dose, consult your healthcare team for guidance. Store insulin and other medications properly. Most insulins should be refrigerated before first use and then stored at room temperature. Never use expired medication. Keep your medication in a cool, dry place, away from direct sunlight. Using the right storage helps to maintain the drug’s effectiveness.
Tip 5: Maintain Consistent Communication with Your Healthcare Team
Maintaining consistent communication with your healthcare team is essential for managing diabetes effectively and extending the honeymoon phase. Regular check-ups, open communication, and actively participating in your care ensure that you receive the best possible support and adjustments to your treatment plan. This proactive approach enables you to stay on track, address any concerns, and make informed decisions about your health. Make sure to be open and honest with your healthcare team about any issues or concerns you are experiencing.
The Value of Regular Check-ups
Regular check-ups with your endocrinologist, primary care physician, and other healthcare providers are critical. During these appointments, your healthcare team will monitor your blood sugar levels, review your medication and treatment plan, and check for any complications. They can also provide guidance and adjust your treatment as needed. These check-ups provide an opportunity to ask questions, discuss any concerns, and get personalized advice. Following the guidance offered by your healthcare providers helps to make sure you stay healthy.
What to Discuss with Your Doctor
Be prepared to discuss your blood glucose readings, any symptoms you are experiencing, and any changes in your lifestyle. Share any concerns you have about your medication, diet, or exercise routine. Ask questions to better understand your diabetes and how to manage it effectively. Bring a list of questions and concerns to each appointment. Keep a detailed log of your blood sugar levels, food intake, and exercise activity to share with your doctor. This communication helps your healthcare team to better assist you.
Coping with the End of the Honeymoon Phase
The end of the honeymoon phase is a natural progression of Type 1 diabetes. As the body’s ability to produce insulin diminishes further, you may notice an increased need for insulin and potentially experience a return of diabetes symptoms. However, by continuing to adhere to the management strategies discussed, you can still maintain good blood sugar control and minimize the impact of diabetes on your life. It is important to work closely with your healthcare team to adjust your treatment plan as needed and to receive ongoing support. Remember, while the honeymoon phase may end, you can still live a healthy and fulfilling life with diabetes.
